Just over three weeks ago, the EHC held two webinars focused on women with rare bleeding disorders looking at the management of heavy menstrual bleeding and access to specialised care for women with rare bleeding disorders.
One of the most recurring questions on these topics is access to treatment and treatment options for women with rare bleeding disorders. Diana Lighezan, a member of the committee and haematologist in training talks us through the various treatment options that are available and may be offered to women with bleeding disorders.
In order to access treatment, one must be diagnosed. How can this happen?
We know that many women in the bleeding disorders community such as mothers, sisters or daughters of someone with haemophilia are likely to also be what we traditionally know as carriers. This means that they carry the genetic mutation impacting the body’s coagulation system. What is less known is that up to 30 per cent of these women may experience also bleeding symptoms such as heavy periods, post-partum haemorrhage, nose bleeds, heavy bleeding during and after surgeries or joint bleeds. This is why it is really important for them to get a diagnosis, ideally before they have their first period. I think that it’s also important to move away from the term ‘carrier’ and start to call women with low levels of coagulation factor VIII and IX patients, like their male counterparts.
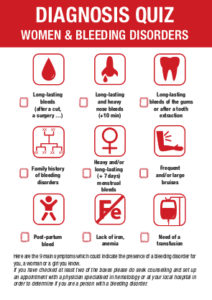
The genetic transmission of other rare bleeding disorders is different and I give you here below some links for further readings. In general, though, I would advise to seek medical help and get diagnosed if:
- Someone in your family has a bleeding disorder,
- You tick yes to two or more symptoms in the bleeding test here below.
The Canadian Hemophilia Society and the World Federation of Hemophilia have a wealth of resources on their website, and we have compiled some here below for you:
If a woman thinks she has a bleeding disorder and wants to get diagnosed, where should she go?
The best option would be to go to a hospital that has specialised healthcare professionals familiar with these disorders. All of these bleeding disorders are rare, which by definition means that they’ll impact less than one in 5,000 people. This means that most healthcare professionals, like general practitioners or gynaecologists, may never even come across someone with a bleeding disorder in their entire career. It is therefore important to go to a specialised centre where healthcare professionals not only know these disorders but have a long clinical practice in treating them, are up to date with the latest research on clinical management and have access to laboratories with the capacity to perform some of the tests that will be used for both the diagnosis and monitoring of the patients’ health. There are usually only a handful of these centres per country and to find them, one can either get in touch with your local patient organisation or also consult the Haemophilia Centre Locator website, which lists most of the specialised haemophilia treatment centres in Europe.
A quick note, although we refer to ‘haemophilia’ treatment centres, these centres are generally also specialised in other bleeding disorders such as Von Willebrand disease, platelet disorders and other rare factor deficiencies.
What treatment options are available for women with bleeding disorders?
 The treatment type you will be offered will depend on your bleeding disorder, its severity and your bleeding phenotype (that is your bleeding pattern). It will also depend on whether the treatment is given to prevent recurring bleeds or to prevent or treat bleeds in a particular situation like a surgery, childbirth or a severe bleed (breakthrough bleed).
The treatment type you will be offered will depend on your bleeding disorder, its severity and your bleeding phenotype (that is your bleeding pattern). It will also depend on whether the treatment is given to prevent recurring bleeds or to prevent or treat bleeds in a particular situation like a surgery, childbirth or a severe bleed (breakthrough bleed).
This article and the treatment options listed below are meant to be informative, and we recommend that readers check-in with a specialised healthcare provider to discuss treatment options adapted to them.
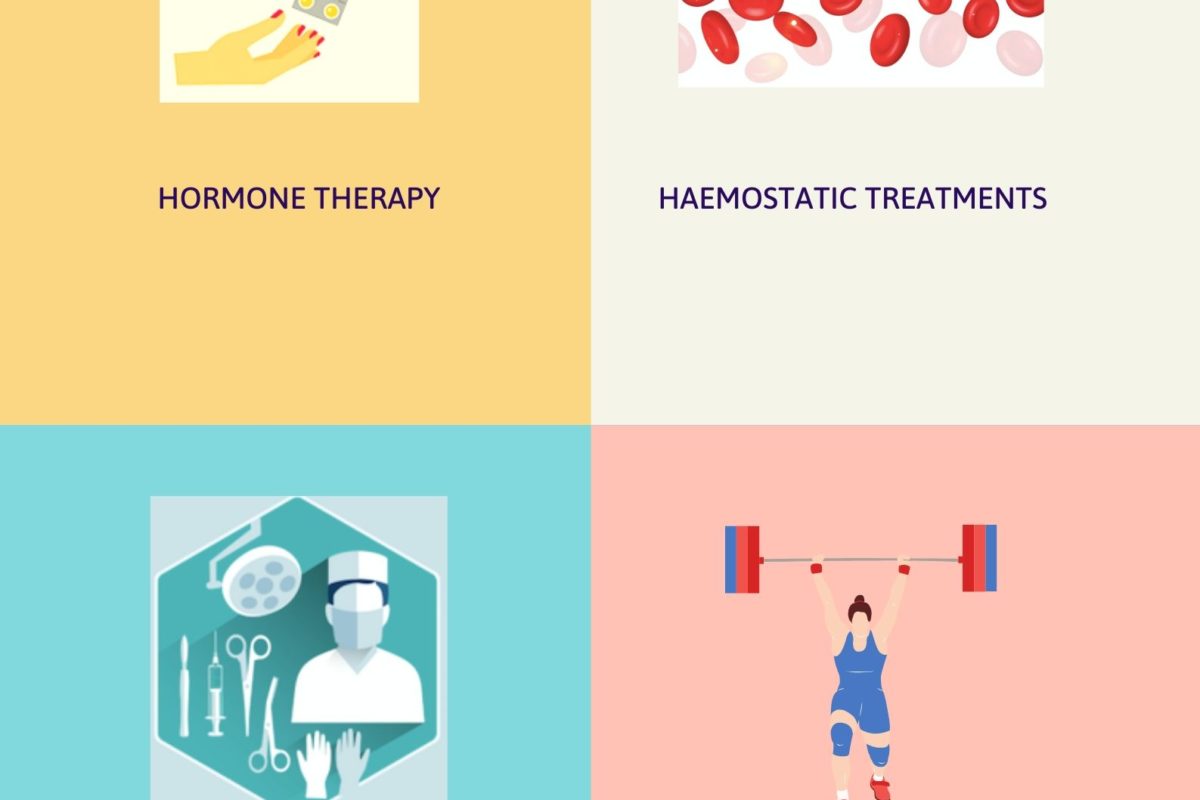
In general, three categories of treatments are used for women with bleeding disorders: hormonal therapy, haemostatic treatment and surgical procedures. In addition to these, your doctor may also prescribe iron supplements, either as a pill or as an injection, for more severe cases. Finally, some women affected by rare bleeding disorders may also require blood transfusions, although this is rarer.
Desmopressin is a synthetic drug, which is a copy of a natural hormone. It acts by releasing von Willebrand Factor (VWF) stored in the lining of the blood vessels. The increased VWF, in turn, transports extra factor VIII. Desmopressin is not made from blood.
Desmopressin is the treatment of choice for Type 1 VWD, haemophilia A carriers and most platelet function disorders. It is sometimes effective in Type 2A VWD.
Desmopressin can be taken in three different ways:
- It can be injected into a vein.
- It can be injected under the skin.
- It can be taken by nasal spray.
Desmopressin is effective for almost all people with Type 1 VWD. However, different people respond to desmopressin in different ways. Therefore, a doctor needs to do tests to find out each individual’s response to the drug. Ideally, these tests are done before any urgent need for the drug, such as surgery.
Since desmopressin acts by releasing VWF stored in the body, you cannot ‘go to the well’ too often. A sufficient amount of time, usually 24 hours, must elapse between doses of desmopressin to allow the body to rebuild its stores.
In major surgery, desmopressin alone may not be enough to control bleeding. In such a case, a person should also receive factor concentrates. (See Clotting factor concentrates)
Desmopressin is of no help to women with:
- Type 2 VWD (except, in some cases, Type 2A)
- Type 3 VWD
- Hemophilia B (factor IX deficiency)
- Glanzmann Thrombasthenia (a type of platelet function disorder).
Source: Canadian Hemophilia Society
Antifibrinolytic agents, like tranexamic acid, are medicines that help to hold a clot in place once it has formed. They act by stopping the activity of an enzyme, called plasmin, which dissolves blood clots.
They do not help to actually form a clot. This means they cannot be used instead of desmopressin, VWF concentrate or factor concentrates.
They can be used to hold a clot in place in mucous membranes such as:
- the inside of the mouth,
- the inside of the nose,
- inside the intestines,
- inside the uterus (the womb).
These medicines have proven very useful for women with bleeding disorders. They are used:
- before dental work
- when a person has a mouth, nose and minor intestinal bleeding
- for women with heavy and /or prolonged menstrual bleeding.
These medicines can even be combined with the use of oral contraceptives for women who do not respond to desmopressin.
Source: Canadian Haemophilia Society
Factor concentrates exist for many of the bleeding disorders that affect women. They replace the missing factor. Factor concentrates can be used:
- when desmopressin, hormone therapy and antifibrinolytic drugs are not effective
- for surgery, or
- after a serious accidental injury.
Factor concentrates are injected into a vein. They can be administered at a clinic, doctor’s office or emergency department. Many people learn to inject them at home.
Source: Canadian Haemophilia Society
The purpose of this surgery is to destroy the lining of the uterus. This is the endometrial tissue, which bleeds so much during menstruation. The operation is done through the vagina and no surgical cutting is needed.
Source: Canadian Hemophilia Society
The purpose of this surgery is to remove the uterus so that menstrual bleeding stops once and for all. This is major surgery and will result in infertility.
Source: Canadian Hemophilia Society
This is a procedure that is done to reduce post-partum bleeding. It consists of a medical device in the shape of a balloon that is inserted (deflated) in the uterus and then filled with saline. This device puts pressure on the uterine wall to stop bleeding. This can be used in conjunction with other antifibrinolytic agents and coagulation factor concentrate.
The purpose of this surgery is to remove endometrial tissue that has formed outside the uterus. This tissue bleeds during menstruation and can cause pain in the pelvis and abdomen. This operation can reduce pain and bleeding in women who do not respond to hormone therapy and other medical treatments.
Source: Canadian Hemophilia Society
This is the removal of the ovaries, and its purpose is to stop bleeding from the ovaries. This is a major surgery that will cause infertility and women will need to take hormones until the age of menopause.
Source: Canadian Hemophilia Society
NOT RECOMMENDED IN WOMEN WITH BLEEDING DISORDERS
The purpose of this surgery is to scrape and clean the lining of the uterus. This is done to diagnose another problem. However, this is not effective in reducing bleeding. It may cause additional bleeding. Also, it may remove any existing platelet plugs and fibrin clots and make the bleeding worse.
Source: Canadian Hemophilia Society
This is a minimally invasive procedure for uterine fibroids, which may cause increased bleeding. The goal is to block the fibroid blood vessels, to stop the blood supply to the fibroid and cause them to shrink and die.




 Jim is aged 66 and has Haemophilia A with a high titer inhibitor which he developed at age 14.
Jim is aged 66 and has Haemophilia A with a high titer inhibitor which he developed at age 14. Maria Elisa Mancuso (MD, PhD) is a Haematologist and works as a Senior Haematology Consultant at the Center for Thrombosis and Haemorrhagic Diseases of IRCCS Humanitas Research Hospital in Rozzano, Milan, Italy. She is Adjunct Clinical Professor at Humanitas University. She obtained a post-degree in Clinical and Experimental Haematology and a PhD in Clinical Methodology. She is involved in clinical research and has published several original articles in peer-reviewed journals a The Lancet, Blood, Journal of Thrombosis and Haemostasis, Haematologica, Thrombosis and Haemostasis, British Journal of Haematology and Haemophilia. She is reviewer for several peer-reviewed journals and member of the Editorial Board of JTH. She is a member of several scientific societies (ISTH, WFH, ASH, EAHAD, SISET, AICE) and was a medical member of the Inhibitor Working Group of the European Hemophilia Consortium. She is co-chair of the ADVANCE Study Group. She has acted also as co-chair of the Scientific and Standardization Subcommittee of ISTH on FVIII, FIX and rare bleeding disorders. She has been involved as principal and co-investigator in several clinical trials, and she takes care of both children and adults with hemophilia and other congenital bleeding disorders with a specific scientific interest in novel therapies, prophylaxis, inhibitors, and chronic hepatitis C.
Maria Elisa Mancuso (MD, PhD) is a Haematologist and works as a Senior Haematology Consultant at the Center for Thrombosis and Haemorrhagic Diseases of IRCCS Humanitas Research Hospital in Rozzano, Milan, Italy. She is Adjunct Clinical Professor at Humanitas University. She obtained a post-degree in Clinical and Experimental Haematology and a PhD in Clinical Methodology. She is involved in clinical research and has published several original articles in peer-reviewed journals a The Lancet, Blood, Journal of Thrombosis and Haemostasis, Haematologica, Thrombosis and Haemostasis, British Journal of Haematology and Haemophilia. She is reviewer for several peer-reviewed journals and member of the Editorial Board of JTH. She is a member of several scientific societies (ISTH, WFH, ASH, EAHAD, SISET, AICE) and was a medical member of the Inhibitor Working Group of the European Hemophilia Consortium. She is co-chair of the ADVANCE Study Group. She has acted also as co-chair of the Scientific and Standardization Subcommittee of ISTH on FVIII, FIX and rare bleeding disorders. She has been involved as principal and co-investigator in several clinical trials, and she takes care of both children and adults with hemophilia and other congenital bleeding disorders with a specific scientific interest in novel therapies, prophylaxis, inhibitors, and chronic hepatitis C. As a patient with factor II deficiency, the diagnostic and treatment of rare bleeding disorders is a matter dear to my heart. My motivation to participate in the work of the ERIN committee is to improve both diagnostic and treatment for patients with rare bleeding disorders across Europe.
As a patient with factor II deficiency, the diagnostic and treatment of rare bleeding disorders is a matter dear to my heart. My motivation to participate in the work of the ERIN committee is to improve both diagnostic and treatment for patients with rare bleeding disorders across Europe. Economist and financial expert by profession, executive coach and trainer by passion and haemophilia advocate by every drop of my blood through my son (who has severe haemophilia A with inhibitors). Bringing a good decade of practical experience from the corporate insurance world, laser focus, growth mindset and resilience from my own experience, offering you anything I can just do, in hope that together we can make life more fulfilled for those impacted by bleeding disorders.
Economist and financial expert by profession, executive coach and trainer by passion and haemophilia advocate by every drop of my blood through my son (who has severe haemophilia A with inhibitors). Bringing a good decade of practical experience from the corporate insurance world, laser focus, growth mindset and resilience from my own experience, offering you anything I can just do, in hope that together we can make life more fulfilled for those impacted by bleeding disorders. Amy Owen-Wyard is a Registered Mental Health Nurse. With experience working with children, young people, their families and adults with severe and enduring mental health conditions. Amy was also involved in a service improvement to provide a holistic care approach for those in general hospitals to support both their mental and physical health, whilst sharing her expertise and knowledge in mental health with the wider multidisciplinary team.
Amy Owen-Wyard is a Registered Mental Health Nurse. With experience working with children, young people, their families and adults with severe and enduring mental health conditions. Amy was also involved in a service improvement to provide a holistic care approach for those in general hospitals to support both their mental and physical health, whilst sharing her expertise and knowledge in mental health with the wider multidisciplinary team.