Bleeding Disorders
The EHC strives both at the European and national levels to increase the awareness and advocate for people with bleeding disorders. This page provides a short overview of what these conditions are and how they affect daily life of patients.

BLEEDING DISORDERS
What are bleeding disorders?
‘Bleeding disorders’ is a generic name for a group of disorders that affect the ability of blood to clot in an individual. Bleeding disorders include conditions such as haemophilia A and haemophilia B, von Willebrand Disease (VWD), and other rare bleeding disorders (RBDs). These conditions present themselves in either severe, moderate or mild forms.
When they have access to adequate treatment, people with bleeding disorders are able to lead normal and fruitful lives. However, limited access to treatment and care can have drastic consequences on the lives of those affected by these conditions. In fact, bleeds that are not properly managed can be crippling and even life-threatening when they occur for example in the brain.
All bleeding disorders fit the description of rare diseases as provided by the European Union, which is a condition that affects less than 1 person in 2,000. Despite being rare diseases, conditions such as haemophilia and von Willebrand Disease (the most frequent bleeding disorders) are ahead of the curve compared to many other rare diseases, in the sense that both diagnostics and a variety of treatments exist for these conditions.
The challenges faced by these patients relate to a lack of access to adequate treatment (which is often expensive) and specialised healthcare services (which may be located only in one or two cities in a given country). Furthermore, patients within the European region face great disparities in access to treatment and, as a result, have different qualities of life.
If you are a patient with a bleeding disorder and you are looking for more in-depth medical information, we recommend the following websites:
- The website of your national haemophilia association
- EHC Academy
- The World Federation of Hemophilia eLearning Platform
- Orpha.net
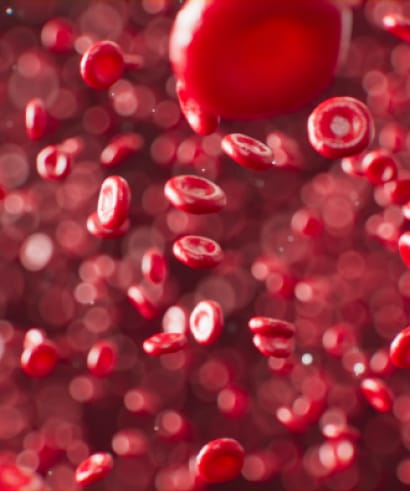
The Clotting Process
Clotting factors are proteins in the blood that control bleeding. When a blood vessel is injured, the walls of the blood vessel contract to limit the flow of blood to the damaged area. Then, small blood cells called platelets stick to the site of the injury and spread along the surface of the blood vessel to stop the bleeding.
At the same time, chemical signals are released from small sacs inside the platelets that attract other cells to the area and make them clump together to form what is called a platelet plug.
On the surface of these activated platelets, many different clotting factors work together in a series of complex chemical reactions (known as the coagulation cascade) to form a fibrin clot. The clot acts like a mesh to stop the bleeding.
Coagulation factors circulate in the blood in an inactive form. When a blood vessel is injured, the coagulation cascade is initiated and each coagulation factor is activated in a specific order to lead to the formation of the blood clot. Coagulation factors are identified with Roman numerals (e.g. factor I or FI) although the coagulation cascade does not follow numerical sequencing.
How coagulation disorders affect an individual
One of the main impacts of bleeding disorders on an individual is the damage to joints such as hips, knees, wrists, ankles, and shoulders.
Joints are part of the body with a high number of blood vessels. They are therefore more at risk of bleeds. When a bleed occurs in the joint, the synovium (which is part of the joint) absorbs the blood in an attempt to remove it. The iron in the blood accumulates in the synovium. Doctors think the iron causes the synovial lining to get thicker. The thicker the synovium is, the more blood vessels it contains. This, in turn, makes subsequent bleeding more likely. This results in similar effects as people suffering from arthritis.
The more bleeds an individual experiences, the more damage is done to the joint. This can lead to joint destruction, leaving the affected individual with very little to no movement range. Besides causing disability, joint bleeds are extremely painful and if not properly managed can take up to several weeks to recover. This can increase days of hospital stay and not being able to take part in any study, work or social activity. This is why it is recommended to prevent joint bleeds instead of treating them.
At the moment it is believed that prophylactic treatment is the best solution to prevent joint bleeds. Unfortunately, this is often seen as an expensive course of action. However, the EHC believes that investing in the prevention of joint bleeds is the optimal course of treatment. In fact, once a joint bleed occurs, the affected individual may receive a high amounts of coagulation factor to stop the bleed and, at the end of the year, this amount of factor may be comparable to treatment levels the individual would have received, had prophylaxis been followed.
Different types of bleeding disorders
Therapy
EHCucate

EHCucate
Learn about all treatment options in our EHCucate project and create your learning path through interaction with different multimedia formats here!
Treatment By Cohort

Treatment By Cohort
Access a cohort-based approach to the licenced-in-the-EU treatment options here!
Treatment Data Set

Treatment Data Set
Access a comprehensive data set about treatment options available in our NMOs (updated periodically) here!
Novel Treatment Review

Novel Treatment Review
Get to know the latest updates in novel treatments, including the drugs in development here!
Treatment Updates

Treatment Updates
Access periodic updates on products, related safety issues, licensing and more here!
Useful information
Here some important things to keep in mind when travelling with a bleeding disorder:
Always take your medical identification information with you, including your last haemostasis results in case of an emergency.
Always carry your own treatment products, treatment equipment, and pharmaceutical drugs with you, as products will be different and probably very expensive in another country. Also, most countries have only limited supplies available and cannot be expected to give products reserved for their own patients to travellers.
Carry a letter for security staff at your port of exit or entry, explaining why you are carrying treatment products, prescribed drugs, needles, syringes etc., and the serious implications of not having them immediately to hand.
When travelling by air, always carry your own treatment products, treatment equipment and pharmaceutical drugs on-board the aircraft as hand baggage. This will allow you to present them quickly to security and customs, if requested. In addition, there are risks of loss, breakage and of temperature variations potentially affecting treatment products if stowed in the aircraft hold.
Carry a letter from your treating doctor with information about your bleeding condition, any blood-borne viruses you may have and the usual treatment you receive. This letter should, if possible, be in the language of the country being visited. You may not always be able to treat yourself so this information is important.
Carry a letter to present to customs, if requested, to explain why you are carrying treatment products, prescribed drugs, needles and syringes. Again, this letter should be in the language of the country being visited.
Before seeking healthcare in another EU country, it’s important to check with your national contact point to confirm which medical expenses are covered by your insurance, particularly for hospital stays or specialized treatments. Generally, medical services abroad are covered only if they are also covered in your home country, with different rules applying for emergencies. For more details on cross-border healthcare, visit the European Commission’s Your Europe website.
Prior to travelling, we recommend checking the Haemophilia Centre Locator application to access information about the centre nearest to you within the shortest delays.
You may wish to write in advance to haemophilia centres in the country you are visiting to enquire about the availability of treatment products and medical expenses that may be incurred for treatment.
National haemophilia organisations [link to Our Membership page] can also be a source of assistance if needed while travelling. If you are travelling outside Europe, we recommend that you consult the Global Treatment Centre Directory of the World Federation of Hemophilia.
If possible, make sure that you have the appropriate travel insurance. It is important to declare your bleeding condition otherwise medical attention related to it may not be covered. Ask your national haemophilia organisation for advice about which insurers to approach.
Stay up-to-date with the latest EHC activities and events!

